Integrated Kidney Care
DaVita® Integrated Kidney Care (IKC) has led the industry in providing coordinated, holistic kidney care for more than two decades, and currently manages the total care for more than 25,000 patients with chronic kidney disease (CKD), of which more than 13,000 have end stage renal disease (ESRD).
During 2018, DaVita IKC provided education, resource support and care coordination to help patients better manage their kidney disease and transition smoothly to dialysis. Through engaging with patients and collaborating with kidney doctors (nephrologists), 75 percent of our patients transitioned to dialysis with a permanent access (a device that can access blood in order to clean it) in place. DaVita IKC outperformed the rest of the industry in early access placement by nearly 100 percent. (1)
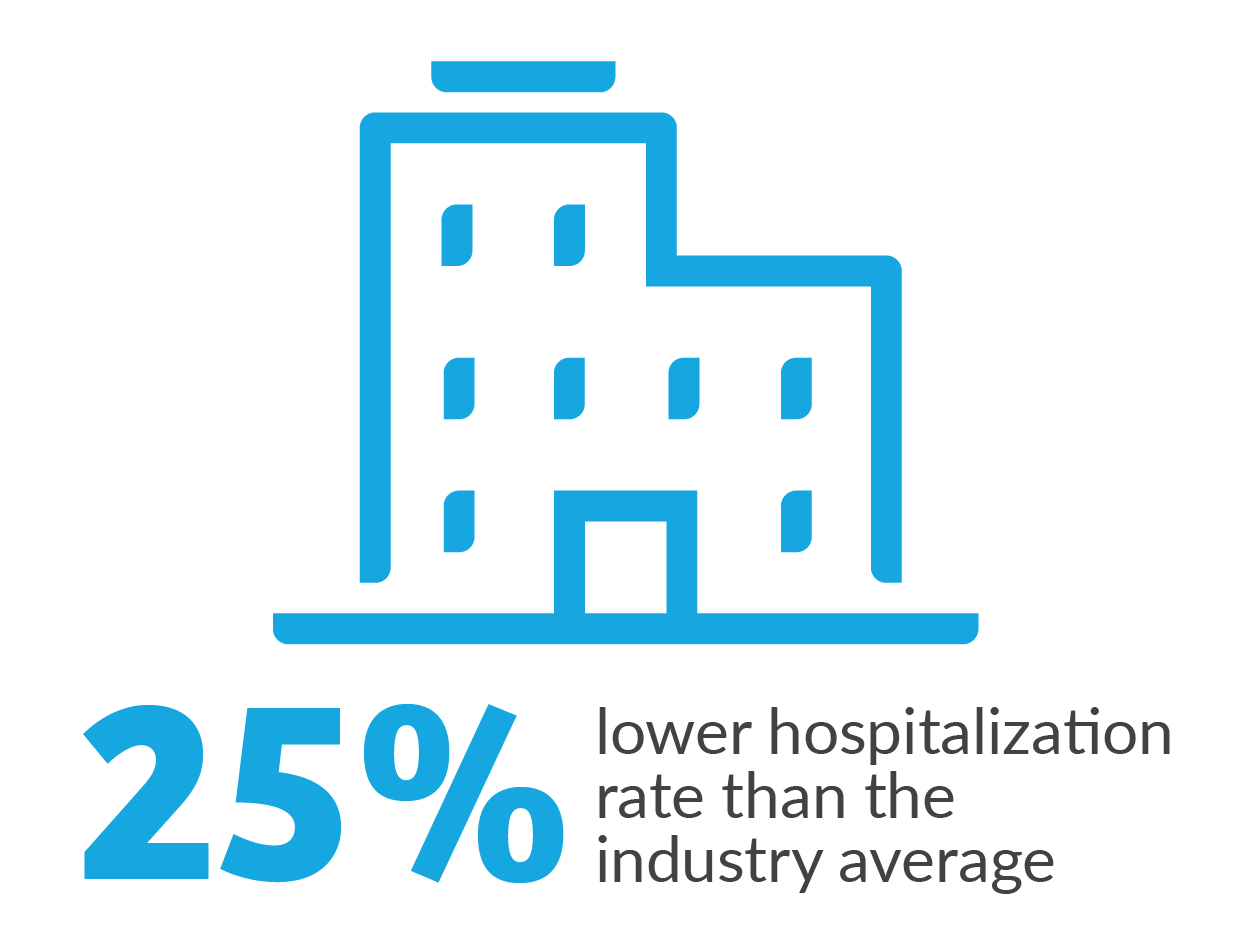
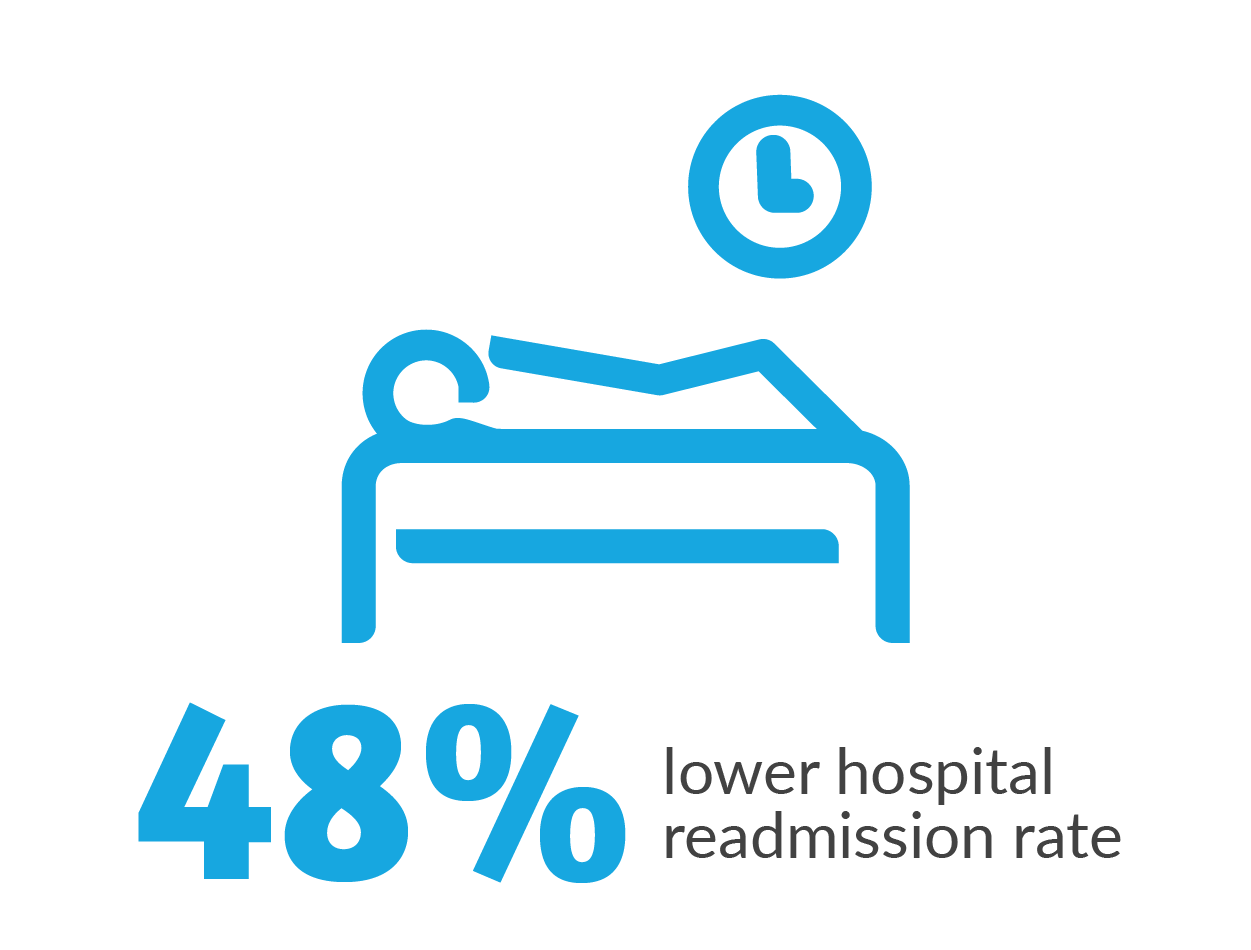
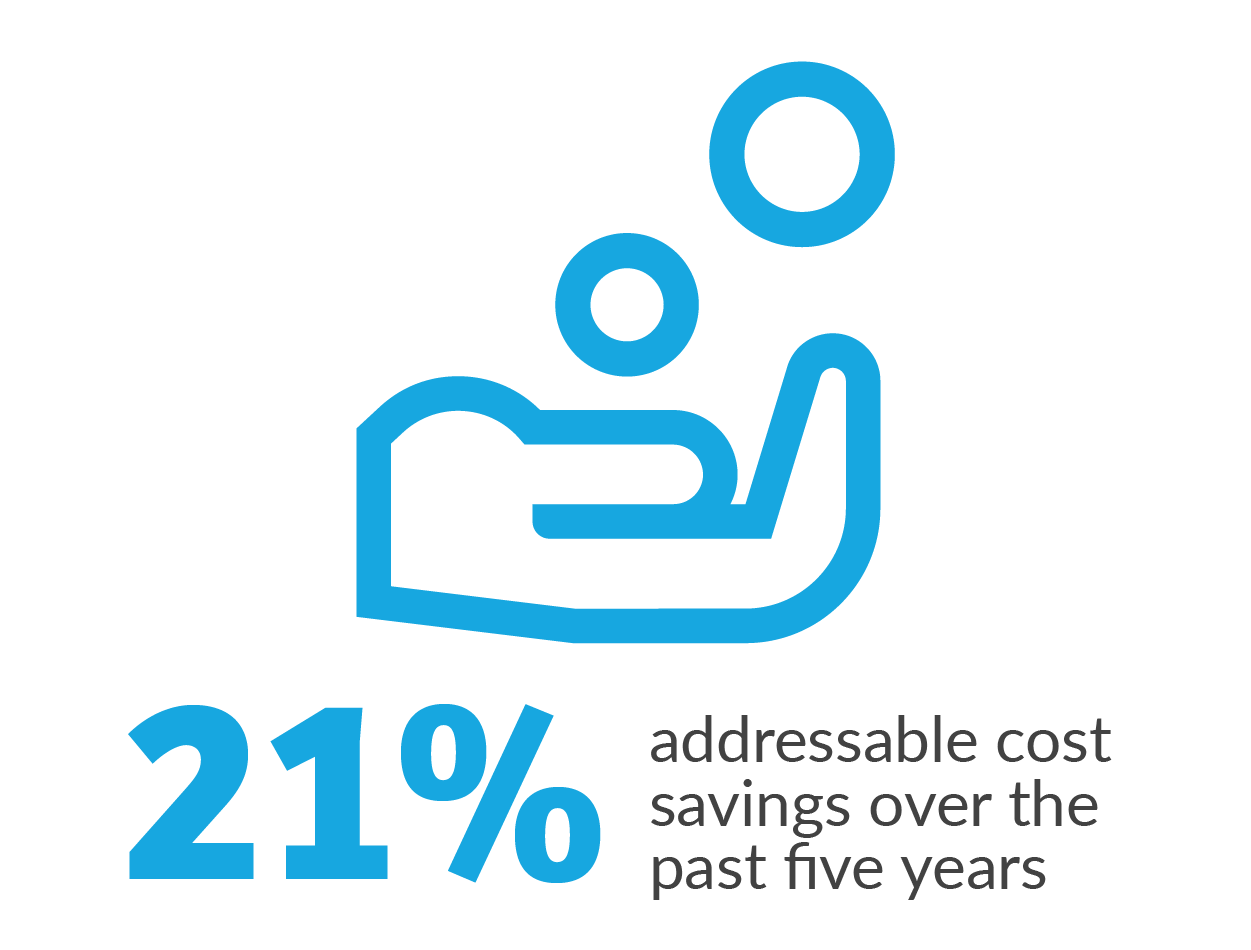
In 2018, our IKC risk-arrangement programs demonstrated compelling results, as shown below. (1)
1. Internal DaVita data. 2018.
Innovating Home Dialysis Care
Dialyzing at home means our patients can have more time for moments with their loved ones while receiving the life-saving treatment they need. When patients dialyze from the comfort of home, they are able to have better control of their treatment schedules, giving them more time for themselves, their families, their jobs, and the activities they enjoyed before starting dialysis.
Patients who perform peritoneal dialysis (PD) at home may have fewer hospitalizations,(1) lower Medicare costs (2) and better transplant outcomes. (3)
DaVita experienced our highest-ever growth year, supporting more than 25,000 patients who dialyze at home—the largest population of home dialysis patients in the U.S. We have 1,500 home dialysis centers across the U.S., (4) which offer support and home dialysis training programs for patients and we’ve grown our home dialysis program nearly four times as fast as our in-center program. (5)
We are advancing and transforming patient care through innovations such as home remote monitoring, telehealth, predictive analytics and other programs to meet patients where they are and help them thrive in the home environment. These technologies also help our care teams deliver the right interventions at the right time to address each patient’s unique clinical needs.
1. Fried L et al. Am J Kidney Dis. 1999 May;33(5):927-933. 2. USRDS 2016 Annual Report. 3. Molnar, MZ et al.Clin J Am Soc Nephrol. 7: 332–341, 2012. 4. Nephrology News & Issues. Sept. 2018. 5. DaVita internal data.
A CHAMPION FOR TRANSPLANT
DaVita’s innovation story is about transforming care across the entire kidney care continuum, from chronic kidney disease (CKD) to transplant, ensuring the right treatment at the right time—something we’ve done for over 20 years.
We believe that kidney transplant is often an ideal treatment option for eligible patients with kidney failure.
Above, watch DaVita Kidney Care patient Dr. Hank Williams talk about why he chose a kidney transplant.
Caring for Our Nation’s Most Vulnerable Patients
DaVita® Health Solutions delivers comprehensive care programs—including house calls, post-acute care and 24/7 care coordination and support —through at-risk arrangements with health plans to manage their high-risk patients who have multiple chronic conditions. For nearly two years, DaVita Health Solutions programs have served approximately 7,000 patients in collaboration with more than 600 local primary care physicians, specialists and extended care teams.
PROGRAM RESULTS WERE EXTREMELY POSITIVE IN ITS FIRST YEAR: (1)
- 35 to 40 percent fewer hospitalizations
- 15 to 20 percent lower cost of care
- 91 percent patient satisfaction rating
1. J. Ryan, M. K. Abrams, M. M. Doty, T. Shah, and E. C. Schneider, How High Need Patients Experience Health Care in the United States: Findings from the 2016 Commonwealth Fund Survey of High Need Patients, The Commonwealth Fund, December 2016.